C-1 9309
Case Reports Potentiation of Haloperidol Neurotoxicity in Acute Hyperthyroidism: Report of a Case Hsin Chu1,2, Jiann-Chyun Lin1, and Yaw-Dong Hsu1 Abstract- Haloperidol has been used extensively for the treatment of many psychiatric illnesses as well as for control of agitated patients. Side effects including anticholinergic, extrapyramidal, sedative side effects as well as neuroleptic
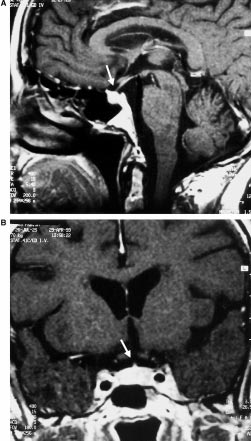 J. Klein et al., Hypophysitis in a 75-year-old woman
Table 1 Pathological blood chemical values at presentation
Corticotropin-Releasing Hormone stimulation. Sim-
ilarly, Thyrotropin-Releasing Hormone stimulation
did not elicit an adequate response of TSH. Finally,
secondary hypogonadism was detected as evidenced
by low FSH and LH baseline levels and the absence
of a significant rise of these hormones after Gona-
dotropin-Releasing Hormone stimulation.
J. Klein et al., Hypophysitis in a 75-year-old woman
Table 1 Pathological blood chemical values at presentation
Corticotropin-Releasing Hormone stimulation. Sim-
ilarly, Thyrotropin-Releasing Hormone stimulation
did not elicit an adequate response of TSH. Finally,
secondary hypogonadism was detected as evidenced
by low FSH and LH baseline levels and the absence
of a significant rise of these hormones after Gona-
dotropin-Releasing Hormone stimulation. Table 2 Results of pituitary function tests at presentation
Plasma hormone levels were measured before (À60, À15), at the time (0), and after (+15, +30, +45, +60, +90) the application of an
intravenous bolus injection of 60 mg CRH, 1.5 mg LHRH, and 12 mg TRH; range of normal values in parenthesis
presentation of 31 years (Beressi et al., 1999; Powrie
et al., 1995). To our knowledge, this is the first report
of a woman 75 years of age presenting with
hypophysitis. Interestingly, we also found elevated
TPO-antibodies in the patient presented. This is in
keeping with previous reports (Barbaro and Loni,
2000; Beressi et al., 1999; Goudie and Pinkerton,
1962; Nagai et al., 1997; Pestell et al., 1990; Sobrinho-
Simoes et al., 1985) and lends support to the
hypothesis of an autoimmune origin of hypophysitis.
Table 2 Results of pituitary function tests at presentation
Plasma hormone levels were measured before (À60, À15), at the time (0), and after (+15, +30, +45, +60, +90) the application of an
intravenous bolus injection of 60 mg CRH, 1.5 mg LHRH, and 12 mg TRH; range of normal values in parenthesis
presentation of 31 years (Beressi et al., 1999; Powrie
et al., 1995). To our knowledge, this is the first report
of a woman 75 years of age presenting with
hypophysitis. Interestingly, we also found elevated
TPO-antibodies in the patient presented. This is in
keeping with previous reports (Barbaro and Loni,
2000; Beressi et al., 1999; Goudie and Pinkerton,
1962; Nagai et al., 1997; Pestell et al., 1990; Sobrinho-
Simoes et al., 1985) and lends support to the
hypothesis of an autoimmune origin of hypophysitis.